
Home Stretch | A balloon in your belly
Computer models and new ultrasound technique improve imaging of abdominal aneurysms
For some patients, living with an aneurysm feels like walking around with a ticking time bomb. Biomedical engineers Judith Fonken and Vera van Hal are working to more accurately visualize such a dilation of the abdominal aorta using computer models and new ultrasound technology. This will enable specialists to make better-informed decisions about which patients should undergo surgery.
If you keep inflating a balloon, it’s only a matter of time before it pops. The balloon will burst apart at the point where the plastic is weakest. And the same thing can happen with an aneurysm, explains Judith Fonken. For the past four years, she and her colleague Vera van Hal have been researching abdominal aneurysms in the Photoacoustics and Ultrasound Laboratory (PULS/e). They refer to these using the professional term Abdominal Aortic Aneurysms (AAA). Their expertise in the field goes back even further, because for both Fonken and Van Hal, this doctoral project is a continuation of their master’s final project. This week, after defending their dissertations, their years-long collaboration will come to an end.
Ticking time bomb
What causes such a weak spot in an (abdominal) artery is not fully understood. However, it is known that high cholesterol, obesity, smoking and male sex are risk factors for developing an aneurysm. The problem is that an aneurysm often causes no health symptoms, so patients walk around with a ticking time bomb without realizing it, Fonken emphasizes. “A vascular surgeon typically considers surgery advisable once the diameter reaches 5.5 centimeters (5 centimeters in women). However, some aneurysms rupture before that threshold, and we’ve also seen a patient with a stable dilation of as much as 16 centimeters.” For comparison: normally, the abdominal aorta has a diameter of about 2 centimeters.
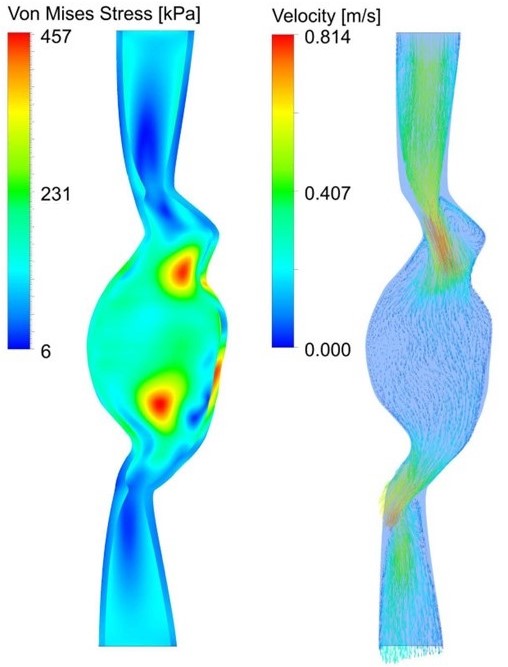
A vascular surgeon wants to make a well-informed risk assessment: when should I operate? A ruptured abdominal aorta carries a high risk of death, but surgery is not entirely without risk either. That is why a patient-specific model and improved imaging are essential, according to Fonken. “We want a better predictor of how an AAA develops. Currently, specialists take a 2D ultrasound image at the point of maximum diameter, but our work shows that properties of the vessel wall can provide a lot of additional information. My aim is to capture that in a model that is useful to the physician.”
What we really want, Van Hal clarifies, is to create a sort of 3D representation of the risk of rupture. “It would show the specific shape of the aneurysm in the patient and indicate where the risk of rupture is highest. And how high that risk is. To do that, we need a different way of visualizing – one that also factors in the strength of the vessel wall and the stresses acting on it.”
A pad on your belly
Patients with abdominal aneurysms are examined several times a year to monitor the growth of the AAA. Fonken: “A CT scan provides a very accurate picture of the entire affected blood vessel, but because of the amount of radiation and the use of contrast medium, you can’t do that repeatedly. Ultrasound is a very safe and accessible alternative.”
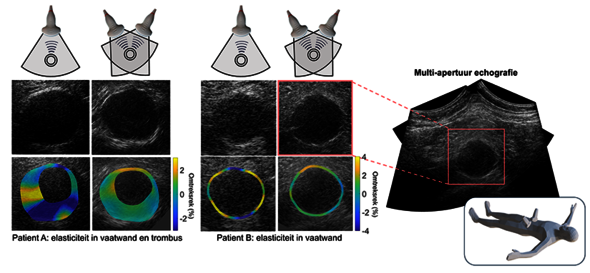
However, current ultrasound images do not show the entire aneurysm. Information about the aneurysm’s sides is often missing, as Van Hal demonstrates using an image in her dissertation. The reason for this is that the sound waves reflect in a different direction there, which prevents them from reaching the ultrasound probe. That is why Van Hal developed a new ultrasound technology that allows her to capture images of the abdominal aneurysm using two probes simultaneously. “We use this to measure from two different angles, which already produces a dramatically improved image. The ultrasound probes are currently fixed in a metal arch, but ultimately, we want to switch to a flexible ultrasound probe that you can place on your abdomen like a pad, allowing signals to be captured from even more directions.”
Fat tissue
What started four years ago with the development of experimental techniques on pieces of pig aortas has now been successfully implemented in clinical practice. “In the clinic, you encounter new practical challenges, such as patients of all shapes and sizes. Sometimes, the large differences in the speed of sound between fat and muscle tissue can cause the individual ultrasound images to shift. I can now correct that with a new method. And sometimes, just pressing down the ultrasound probe a little harder is enough too.”
In addition to achieving better image quality with a higher frame rate – the number of images per second has increased from 30 to 130-180 per second – and visualizing parts of the vessel wall that were previously not visible, Van Hal can now also determine the local elasticity of the vessel wall.
Fonken plans to eventually incorporate this information into her computer model, which she initially set up using current patient data. “The direct stretching of the vessel wall can’t be measured in patients with current techniques, but we can simulate it using a biomechanical model. With the new ultrasound techniques, we can actually measure this local stretching and use it as input for this model. This will ultimately allow us to determine the patient-specific material properties of the aneurysm. We can then translate the combination of wall tension and wall strength into a rupture index which will indicate the risk of rupture and show the differences between patients in terms of growth rate depending on location of the aneurysm.”
Blood clots
In addition, Fonken also examined the role of blood clots adhered to the vessel wall, something that doctors currently have little regard for. “Such an intraluminal thrombus (ILT) occurs in 75% of patients with an aneurysm. The contrast of an ILT is low, which is why they often remain unseen. Vera’s work makes the ILT more visible and we can also use it to determine its elasticity. That could provide a lot of valuable scientific information,” says Fonken enthusiastically.
Because there is still a lot we don’t know about these ILTs, she continues. “We see that blood clots affect blood flow – and vice versa, which complicates things – and rupture risk. In patients without an ILT, a specialist can predict fairly well how fast the aneurysm will grow based on its diameter. With an ILT, this is much more complex; and we’ve shown that a simple ratio is no longer sufficient in that case. This makes it all the more important to use a patient-specific model. That gives the physician more insight and can hopefully prevent unpleasant surprises. The less ‘out with a bang,’ the better.”
PhD in the Picture | Judith Fonken
What is that on the cover of your dissertation?
“A friend drew a schematic of an aneurysm. In it, you see gears symbolizing wall mechanics and lines symbolizing flow profiles. Or you could see it as a ticking clock.”
You’re at a birthday party. How do you explain your research in one sentence?
“That we can provide a better indication of which patients with an aneurysm need surgery based on ultrasound imaging and computer models, and to do that, we must first better understand aneurysm growth.”
How do you blow off steam outside of your research?
“Out with the animals. Walking the dogs, but mostly spending time with my horses. Going for rides outside, practicing dressage in the arena – though I’m currently not competing due to the birth of a foal. But also just mindlessly mucking out stables, turning my brain off for a moment.”
What tip would you have liked to receive as a beginning PhD candidate?
“Take a critical look at the group you’re joining. Of course the research topic should interest you, but supervision and workload are just as important for successfully completing your PhD. I was fortunate to have a great group of people around me.”
What is your next chapter?
“As of May 1, I’m starting a new job at Philips, where I’ll be working on medical imaging as a product tester.”
PhD in the Picture | Vera van Hal
What is that on the cover of your dissertation?
“A mountain landscape – I love nature – with the two mountains representing the two ultrasound probes and the landscape in the foreground resembling a pressed belly. The line art represents the propagation of sound waves.”
You’re at a birthday party. How do you explain your research in one sentence?
“I improve the quality of ultrasound images to make an aneurysm more visible so that we can extract further information about the elasticity and strength of the vessel wall from those images.”
How do you blow off steam outside of your research?
“By dancing! I practice hip-hop a lot at Footloose, where we also create our own choreography with our crew. Although I’ve barely had any time for that in the past six months. Because I had a dissertation to complete, but also because of my wedding and honeymoon in Thailand.”
What tip would you have liked to receive as a beginning PhD candidate?
“I agree with Judith’s tip. Supervisors and colleagues can make or break your PhD track.”
What is your next chapter?
“I really enjoy doing research and have my eye on a postdoc position in New Zealand. Also in the field of ultrasound, but with a stronger focus on practical application.”



Discussion